| Table of Contents |
|---|
Process Group
Claims Management
...
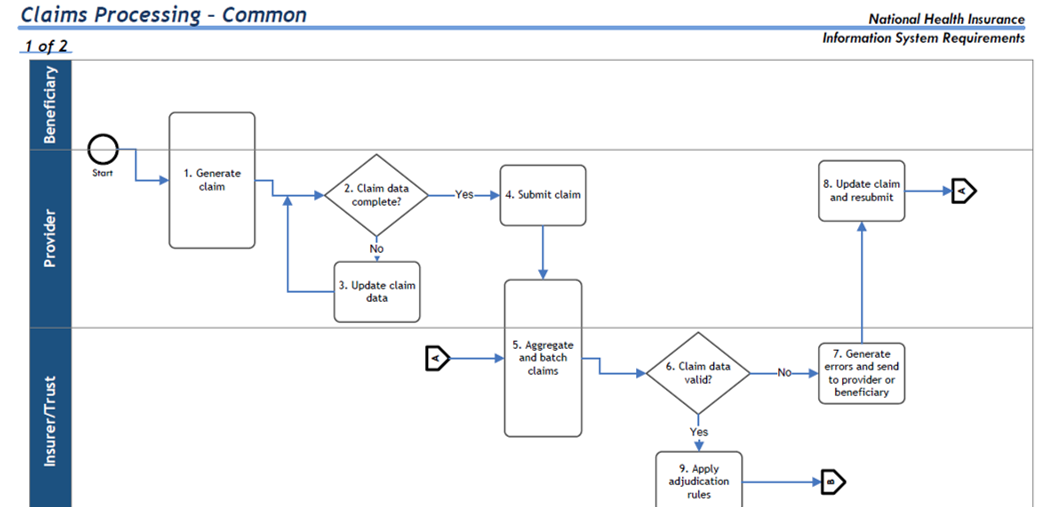
Timely and accurate processing of claims to determine the validity of the claim and the amount to be paid.
Input
Beneficiary identifier
Adjustments
Voids
Re-submitted claims
Pre-authorization match
Eligibility status
Benefit class
Beneficiary accumulators
Provider accumulators
Output
Claim identifier
Claim status (in process, partially approved, approved, rejected, requires more information, in medical review)
Amount approved for claim
Financial transaction to GL
Update beneficiary accumulators
Update provider accumulators
Line items for claims advice
Task Set
Registration of incoming claim
Assign claim identifier
Pre-process and edit claim data
Manage claims exceptions
Apply adjudication rules (skip to approve or reject)
Flag for fraud and abuse
Route for medical review
Approve and prepare payment transaction
Reject and assign reason code
Update beneficiary and provider accumulators
Determine line items for claim (confirm for proper term: advice, Explanation of Benefits statement, receipt, remittance)
Measurable Outcomes
Claim assigned status and determination of payment
Claims status sent to provider, beneficiary and other appropriate authorities, Explanation of Benefits sent to provider and/or beneficiary
First time claim pass rate
Task Flow Diagram
...