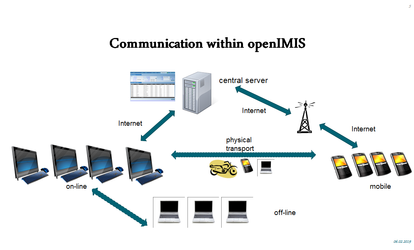
The description of the system for a Health insurance implementation can be done in the following way:
1.Provide an overview of the data flow
Points to cover:
- Centralized server where application resides
- Offline application installed on computers - They are not a replacement for the online application but complements it by enabling entry of new enrolments and submission of claims for insurance staff and health facility respectively to ensure activities do not stop due to internet outages.
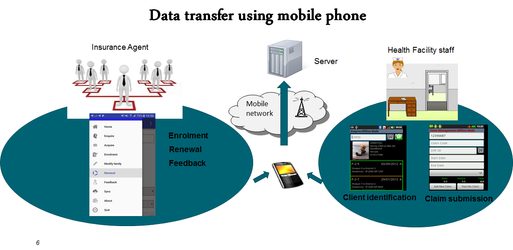
- Mobile phone application - Used by enrolment agents to undertake enrolments, renewals and feedback collection and by health facility staff to undertake client identification and claims submission.
- Data synchronization - Stored data from the offline application installed on a computer as well from the mobile phone application when used offline, can be extracted, physically transported to a location where internet is available and then uploaded to the online application.
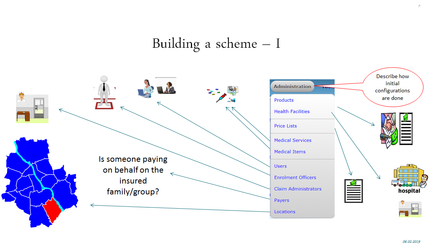
2. Describe how a scheme is constructed (configuration of registers)
Points to cover:
- Creations of Locations - Configured to indicate geographical coverage of the scheme and allocate appropriate access to different users in the system. Currently there can be up to four sub levels defined to indicate geographical boundaries (for eg. Regional -> District -> Municipality -> Village).
- Payers - Configured to indicate a 3rd party payer who would pay the due policy amount on behalf of an insured unit.
- Claims administrator - The personnel responsible at a health facility who is authorized to submit claims on behalf of the health facility.
- Enrolment Officers - The personnel (enrolment officer/agent) responsible for enroling and renewing families/enrolled units.
- Users - Different actors involved in processing data of the insurance scheme are configured here. All users created are given a location and a role according to the function they need to perform in the system.
- Medical Items - A universal list of all possible medical items are configured. These form the basis of establishing facility specific price lists.
- Medical Services - A universal list of all possible service packages are configured. These form the basis of establishing a facility specific or facility type/group specific price lists.
- Price Lists (Medical Service and Medical Items) - A facility specific list of medical services and items are configured. These could be a price list offered by one facility or a type of facilities (eg. all dispensaries) or a groups of facilities (eg. all government facilities). These are based on the price lists negotiated by the insurance scheme.
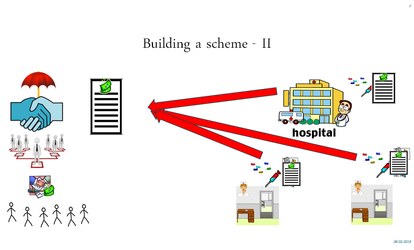
- Health Facilities - A list of contracted health facilities can be configured. These include all different levels of facilities (primary, secondary or tertiary levels) as well the link to respective price lists agreed with the insurance scheme.
- Products - A list of all insurance products on offer by the health insurer can be configured. The product includes the conditions it applies to the customer as well as to the health facility. These include different provider payment mechanisms (eg. capitation with adjusters, fee for service, service packages, etc.) and limits like ceilings per event, per individual or per family as well co payments etc. A health insurer can have one or multiple products and can offer it either in all locations or restrict them by location.
3. Describe how operations are handled structured by key processes
3.a. Enrolment Process
- Using web application
- Using mobile application
Enrolment app login:
EO code: E00005
Login name: sidsri
Password: sidsri2019
3.b. Health service utilization
Enquire ID: 174000002
- Using web application
- Using mobile application
3.c. Claims process
Claims Submission
- Using web application
- Using mobile application
Claims Verification
Claims Payment
HF Code: RAHOSOO1 (Rapta District Hospital)
Claim Admin Code: RHOSOO11 (Rijo Lawrence)
Claim Admin Login ID: rijo
Claim Admin Login password: rijo2019
Service: A1 Consultation - I unit
Item: 0176 ORAL REHYDRATION SALTS (ORS) FOR 1 LITRE POWDER - 2 Unit
Visit Date To & Visit Date From: Same (outpatient - approved, eg. Claim ID RAH00001) or different (inpatient - rejected, eg. RAH00002)